
Capital Blue Cross (CBC):
1-833-584-1828

Annual Required Notices
Disaster Relief Ending Notice
On March 1, 2020, in response to the COVID-19 pandemic, the federal government provided a Disaster Relief Period during which group health plans had to extend certain plan deadlines, including special enrollments, COBRA elections and payments, disability plan determination periods, and claims filing, appeals and review periods.
The Disaster Relief period ended on February 28, 2021. Therefore, the deadlines for previously extended actions have now resumed. Please review the following notice and contact the Benefits Department by email with any questions: LGH-Benefits@pennmedicine.upenn.edu
Click Here to Review the Disaster Relief Notice
Medicare Part D Creditable Coverage
Employees age 63 and older who are participating in the LG Select or LG Consumer plan, please read the notice carefully and keep it where you can find it, as you may need to present this to Medicare at some time in the future. This notice contains information regarding your current prescription drug coverage with LG Health/Penn Medicine and prescription drug coverage available for people with Medicare, or soon to become eligible. It also explains the options you have under Medicare prescription drug coverage and can help you decide whether or not you want to enroll. There is no action required from you at this time, this information is for your records only. At the end of this notice is information about where you can get help to make decisions about your prescription drug coverage.
Below are links to the 2024 Notices:
LGH Medicare Part D Creditable Coverage 2024
Summary Annual Reports
Lancaster General Health distributes Summary Annual Reports for the benefit plans it offers to participants annually. These documents contain financial and related plan information that is filed with the Employee Benefits Security Administration, U.S. Department of Labor as required under the Employee Retirement Income Security Act of 1974 (ERISA).
Below are links to the 2022 & 2023 Summary Annual Reports:
LG Flexible Benefit Plan
LG Employee Life Insurance Plan
LG Employee Medical Benefits Plan
LG Employee Long Term Disability
LG Employee Short Term Disability
LG Employee 403b Plan
LG Employee 401k Plan
Annual Funding Notice
Special Enrollment Rights
Federal law allows for special enrollment rights to permit you to elect coverage or add dependents. This would occur in the case of marriage, birth, adoption, or placement for adoption of a child, or loss of other coverage. However, you must provide written notice to the Human Resources/Benefits Department within 31 days of the marriage, birth, adoption, or loss of other coverage to elect benefit(s) coverage.
- For marriage, coverage will take effect on the date of the event.
- For birth or adoption, coverage will be made retroactive to the date of the event.
If you decline enrollment for yourself or your dependents (including your spouse) because of other health benefit coverage, you may be able to enroll yourself or your dependents in LG Health’s plans in the future, provided that you request enrollment within 30 days after your other coverage ends.
Special enrollment can be requested only after losing eligibility for the other coverage, after employer premiums for the other coverage stops, or after exhausting COBRA coverage in effect, when you declined coverage. An individual does not have special enrollment rights if the loss of coverage is the result of the failure to pay premiums or if employment is terminated for gross misconduct reasons.
Women’s Health and Cancer Rights Act
The Women’s Health and Cancer Rights Act requires that group Health Plans provide the following services to any person receiving benefits in connection with a mastectomy:
- Reconstruction of the breast on which the mastectomy has been performed;
- Surgery and reconstruction of the other breast to produce a symmetrical appearance; and
- Prostheses and treatment of physical complications of all stages of a mastectomy, including lymphedemas (swelling associated with the removal of lymph nodes)
If you receive benefits from a Health Insurance Plan for a mastectomy and you then elect to have reconstructive surgery, the Plan must provide coverage in a manner determined in consultation with the attending physician and the patient. The benefits for breast reconstruction and related services will be the same as the benefit that applies to other services covered by your Plan. It is important to note that the Plan covers these expenses and the law requires that we provide this notice each year.
Newborns’ and Mothers’ Health Protection Act of 1996 (NMHPA)
Group health plans generally may not, under Federal law, restrict benefits for any hospital length of stay in connection with childbirth for the mother or newborn child to less than 48 hours following a vaginal delivery, or to less than 96 hours following a cesarean section.
However, Federal law generally does not prohibit the mother’s or newborn’s attending provider, after consulting with the mother, from discharging the mother or her newborn earlier than 48 hours (or 96 hours as applicable). In any case, Plans and issuers may not, under Federal law, require that a provider obtain authorization from the Plan or the issuer for lengths of stay of less than 48 hours (or 96 hours).
The Children’s Health Insurance Program Reauthorization Act (CHIPRA)
Employees and dependents who were eligible for health care coverage in the LG Consumer or LG Select Plan, but are not enrolled, will be permitted to enroll in the plan if they lose eligibility for Medicaid or CHIP (Children’s Health Insurance Program) coverage or become eligible for a premium assistance subsidy under Medicaid or CHIP.
Individuals must request coverage within 60 days of the loss of Medicaid or CHIP coverage or the determination of eligibility for a premium assistance subsidy.
CHIPRA (Children’s Health Insurance Reauthorization Act of 2009) allows states to offer eligible low income children and their families a premium assistance subsidy to help pay for employer-sponsored coverage.
If you have questions regarding CHIPRA, please do not hesitate to contact the Lancaster General Health Benefits Team at 717-544-1177.
Health Insurance Portability and Accountability Act (HIPAA)
This summary provides only a brief overview of the LG Consumer and LG Select Plans’ health privacy practices.
LG Health has issued a Health Privacy Notice that describes how health information about you may be used and disclosed by the LG Health Plans and how you can get access to your information. You should keep a copy of the Health Privacy Notice you received and review it carefully because it describes the Plans’ privacy practices in more detail.
How the Health Programs Will Use Your Information
The Health Plans may use, share, or disclose the personal health information they create, receive, or maintain about you (“protected health information”) for purposes relating to the payment of medical insurance, operation of the Plans, or treatment by a health care provider. The Plans may use or disclose your information in other special circumstances described in the Health Privacy Notice. For any other purpose, the Plan requires your written authorization for the use or disclosure of your protected health information.
Your Individual Rights
You have the right to inspect and copy certain protected health information, request an amendment of the information, request restrictions on the use and disclosure of the information, request that communications be made to you through alternate means or at an alternative location, and obtain an accounting of the information that a Plan has disclosed (with certain notable exceptions, including disclosures for treatment, payment, or certain operational purposes, as well as disclosures to you or disclosures that you authorize). There are certain limitations on these rights as explained in the original Health Privacy Notice.
Questions and Concerns
If you would like more information about the Plans’ privacy practices, or if you feel that your protected health information was mishandled or your privacy rights under HIPAA were violated, you may contact the LG Health Plans HIPAA Privacy Officer at 717-544-4578.
If you believe your privacy rights have been violated, you can file a formal complaint with the LG Health Plans HIPAA Privacy Officer or with the U.S. Department of Health and Human Services Office for Civil Rights at 1-800-368-1019. You will not be penalized for filing a complaint.
You may also make a written request to inspect, copy, or amend protected health information—or for an accounting of disclosures—and submit it to the LG Health Plans HIPAA Privacy Officer. To request an additional paper copy of the detailed Health Privacy Notice, contact the LG Health Plans HIPAA Privacy Officer.
HIPAA Notice and Forms:
HIPAA Privacy Notice
Privacy Notice Election Change Form
Authorization To Use PHI Form
Request to Amend Disclosures of PHI Form
Request to Restrict Disclosures of PHI Form
Request to Access Disclosures of PHI Form
HIPAA Complaint Form
Notice of Health Care Marketplace
At Lancaster General Health, we strive to provide our employees and their dependents with quality health insurance. Key provisions of the Patient Protection and Affordable Care Act (PPACA) require us to provide you with this Notice to inform you of our compliance with the law and to make you aware of your options in the Health Insurance Marketplace.
What We Have Done to Ensure Compliance with PPACA
As a result of the PPACA, several new legal requirements apply to group health plans offered by many employers. These include:
- Minimum value thresholds for healthcare coverage provided (i.e. the portion of covered benefits that the plan pays); and
- Affordable coverage standards (i.e. the portion of coverage paid for by the employer)
We have worked to ensure that the plans we offer meet these standards established by the new law. Our goal is to continue to have employee contributions for employee only coverage that will not exceed 9.86% of the employee’s annual gross earnings and the plan’s share of the total allowed benefit costs covered by the plan, will be no less than 60% of those costs.
The Marketplace
Although our group health plans offer quality insurance at affordable rates, we recognize that some employees may want to explore other insurance options on the “Marketplace” or “Exchange”. This next section will provide a description of the Marketplace and how participating in it may affect your rights under our health plan, so that you may weigh your options.
What is the Health Insurance Marketplace?
The Marketplace is designed to help individuals find health insurance that meets their needs and fits their budget. The Marketplace offers “one-stop shopping” to find and compare private health insurance options. Individuals may also be eligible for a new kind of tax credit (if certain criteria are met) that can lower their monthly premium for coverage purchased through the Marketplace.
Can Someone Save Money on Health Insurance Premiums in the Marketplace?
Individuals may qualify for tax credits that will enable them to save money and lower monthly premiums for coverage purchased through the Marketplace, but only if their employer does not offer coverage, or offers coverage that doesn’t meet certain standards. As noted above, we have worked to ensure that the plans we offer meet these standards established by the new law. Therefore, we do not believe that our benefit eligible employees will qualify for tax credits to purchase coverage in the Marketplace. For individuals who qualify, the amount of their tax credit will depend on household income.
Does Employer Health Coverage Affect Eligibility for Premium Savings through the Marketplace?
Yes. If an individual’s employer offers health coverage that meets certain standards, the individual will not be eligible for a tax credit through the Marketplace and may wish to enroll in the employer’s health plan. However, tax credits that lower monthly premiums or a reduction in certain cost-sharing may be available if an employer does not offer coverage at all or does not offer coverage that meets certain standards. If the cost of an employer’s plan for individuals only (and not any other members of their family) is more than 9.86% of an employee’s household income for the year, or if the employer-provided coverage does not meet the “minimum value” standard set by the PPACA, an individual may be eligible for a tax credit.
Note: If you purchase a health plan through the health insurance Marketplace instead of accepting health coverage that we offer, then you will lose employer contributions to the employer offered coverage. Also, you will not be able to participate in the plan until the next open enrollment period, unless a qualifying life event occurs.
For More Information
For more information about your coverage offered by your employer, please check your Summary Plan Description, Summary of Benefits and Coverage, or contact the HR Benefits department at (717) 544-1177.
For more information on the Marketplace, including your eligibility for coverage through the Marketplace and its costs, visit HealthCare.gov. Information available there includes an online application for health insurance coverage and contact information for a Health Insurance Marketplace in Pennsylvania.
Form 1095-C
The IRS will use the information provided on Form 1095-C to determine whether an employer complies with the “Employer Mandate” requirement under the Patient Protection and Affordable Care Act (“PPACA”). Under PPACA, we must either offer health insurance coverage, or we could be required to pay a penalty to the IRS. This is often called the Employer Mandate. Because of the Employer Mandate, we must file a form with the IRS called Form 1095-C. The IRS will also use the information provided on Form 1095-C to determine who is eligible for a premium tax credit for coverage purchased through the Marketplace.
Similar to the requirement that we offer coverage or face a penalty under PPACA, individuals who don’t purchase their own health insurance coverage must pay a penalty to the IRS unless they fall within an exception. This is called the Individual Mandate.
The information provided on Form 1095-C, Part III contains information that allows the IRS to determine whether you and your family members have complied with the Individual Mandate or whether you could be subject to a penalty. The Tax Cuts and Jobs Act repealed the Individual Mandate, but not until January 1, 2019. So, you must comply with the Individual Mandate during 2018.
Employee Rights and Responsibilities Under the Family and Medical Leave Act (FMLA)
Basic Leave Entitlement
Eligible employees may take up to 12 workweeks of leave in a 12-month period for one or more of the following reasons:
- The birth of a son or daughter or placement of a son or daughter with the employee for adoption or foster care;
- To care for a spouse, son, daughter, or parent who has a serious health condition;
- For a serious health condition that makes the employee unable to perform the essential functions of his or her job; or
- For any qualifying exigency arising out of the fact that a spouse, son, daughter, or parent is a military member on covered active duty or call to covered active duty status.
An eligible employee may also take up to 26 workweeks of leave during a “single 12-month period” to care for a covered servicemember with a serious injury or illness, when the employee is the spouse, son, daughter, parent, or next of kin of the servicemember. The “single 12-month period” for military caregiver leave is different from the 12-month period used for other FMLA leave reasons.
Under some circumstances, employees may take FMLA leave on an intermittent or reduced schedule basis. That means an employee may take leave in separate blocks of time or by reducing the time he or she works each day or week for a single qualifying reason. When leave is needed for planned medical treatment, the employee must make a reasonable effort to schedule treatment so as not to unduly disrupt the employer’s operations. If FMLA leave is for the birth, adoption, or foster placement of a child, use of intermittent or reduced schedule leave requires the employer’s approval.
Under certain conditions, employees may choose, or employers may require employees, to “substitute” (run concurrently) accrued paid leave, such as sick or vacation leave, to cover some or all of the FMLA leave period. An employee’s ability to substitute accrued paid leave is determined by the terms and conditions of the employer’s normal leave policy.
Notice of Nondiscrimination
Affordable Care Act Section 1557 Notice
Lancaster General Health/Penn Medicine complies with applicable Federal civil rights laws and does not discriminate on the basis of race, color, national origin, age, disability, or sex. LG Health/Penn Medicine does not exclude people or treat them differently because of race, color, national origin, age, disability, or sex.
LG Health/Penn Medicine:
- Provides free aids and services to people with disabilities to communicate effectively with us, such as qualified sign language interpreters and written information in other formats (large print, audio, accessible electronic formats, other formats).
- Provides free language services to people whose primary language is not English, such as qualified interpreters and information written in other languages
If you need these services, contact Laura Tobin at 717-544-2696.
If you believe that LG Health/Penn Medicine has failed to provide these services or discriminated in another way on the basis of race, color, national origin, age, disability, or sex, you can file a grievance with:
Laura Tobin, Benefits Manager
555 N Duke Street, PO BOX 3555
Lancaster, PA 17604
717-544-4578, Fax 717-544-1351
Or email at Laura.Tobin@pennmedicine.upenn.edu
You can file a grievance in person or by mail, fax, or email. If you need help filing a grievance, Laura Tobin is available to help you.
You can also file a civil rights complaint with the U.S. Department of Health and Human Services, Office for Civil Rights, electronically through the Office for Civil Rights Complaint Portal, available at https://ocrportal.hhs.gov/ocr/portal/lobby.jsf, or by mail or phone at:
U.S. Department of Health and Human Services
200 Independence Avenue, SW
Room 509F, HHH Building
Washington, D.C. 20201
1-800-368-1019, 800-537-7697 (TDD)
Complaint forms are available at http://www.hhs.gov/ocr/office/file/index.html.
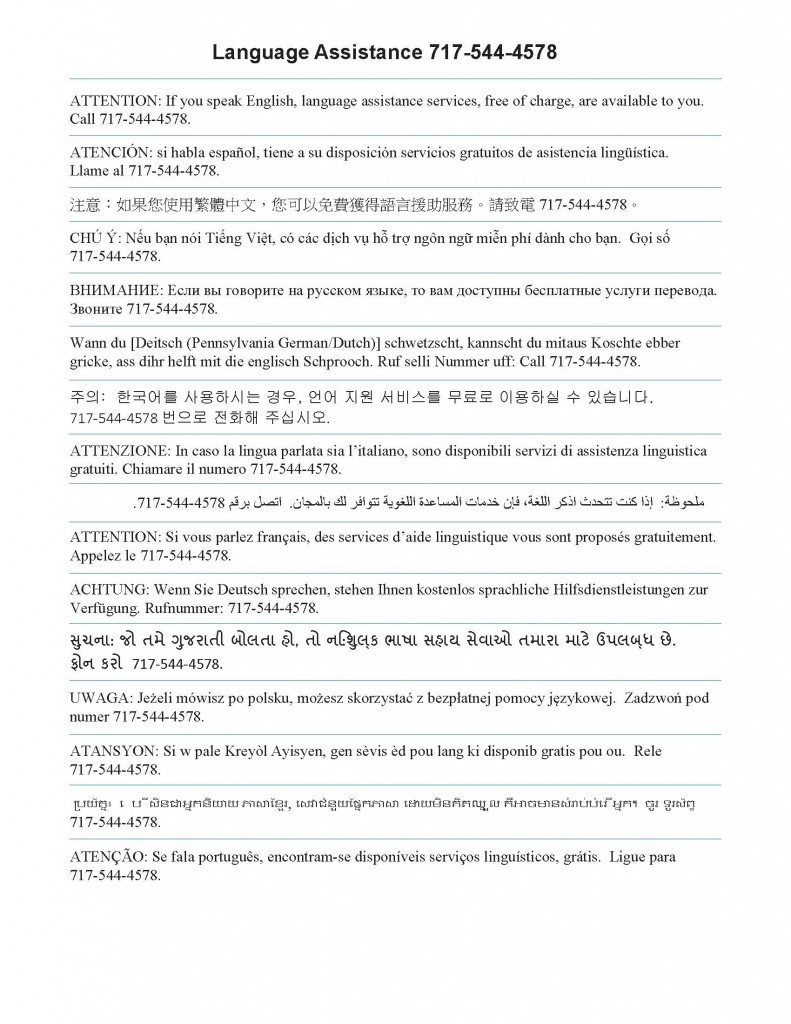
Language Assistance: 717-544-2696
